- Received November 30, -0001
- Accepted November 30, -0001
- Publication December 16, 2019
- Visibility 1 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijcbr.2019.118
-
CrossMark
- Citation
Can GGT and LDH be indicators of endothelial vascular damage in Preeclampsia?
- Author Details:
-
Vanishree B *
-
C D Dayanand
-
Sheela S R
Introduction
Preeclampsia is a maternal syndrome with the symptoms such as hypertension, proteinuria, and edema after 20th weeks of pregnancy.[1] The symptoms of preeclampsia include persistent headache, blurred vision, vomiting, and abdominal pain.[2] It may complicate the pregnancy by leading to fetal uterine growth restriction, preterm delivery, maternal and fetal morbidity and mortality.[3],[4] Preeclampsia is a leading cause of hypertension and complicates up to 10% of the pregnancy.[5] In the hypertensive disorders, preeclampsia and eclampsia have huge impact on the maternal and fetal morbidity and mortality. In Indian scenario, preeclampsia and eclampsia accounts for 24% of the maternal deaths.[6] The incidence of preeclampsia alone in India is reported to be 8-10% among the pregnant women. It usually occurs during the second half of the pregnancy. Pre-eclampsia is more common in primigravida women than the second or later pregnancies.[7]
Although exact cause of preeclampsia is unknown, evidences on placenta playing a role in the pathophysiology have become significant. Shallow endovascular cytotrophoblast invasion in spiral arteries, inappropriate endothelial cell activation and an exaggerated inflammatory response are key features in the pathogenesis of preeclampsia.[8] Pathological placental specimen in preeclampsia shown infarcts by ischemia, occlusion of spiral arteries and failure of vascular remodeling of spiral arteries by trophoblastic cells. This is life threatening for mother and fetus by vasospasm, endothelial dysfunction and ischemia. As a consequence of possible etiological factors, several disturbances in the mother is reason for preeclampsia, which includes changes in hemodynamic, cardiovascular, hematological, endocrine, liver, kidney functions, cerebrovascular, neurological and visual activity.[9]
Serum lactate dehydrogenase (LDH) and serum gamma glutamyl transferase (GGT) have no metabolic functions in the extracellular space. But its level indicates the disturbance. Altered endothelial function play important role in pathogenesis of preeclampsia. Intra cellular enzyme such as LDH increased in serum of preeclamptic women due to cellular death. It is also used to assess the presence of tissue damage. GGT present in many tissues particularly in liver.[10]
Objective of the study was to determine serum lactate dehydrogenase and serum gamma glutamyl transferase as biochemical markers in preeclamptic pregnant women and its comparison with normal pregnant women in third trimester. Also, to find the role of Hb in preeclampsia.
Materials and Methods
Study designed was o bservational prospective case control which was confined to R L Jalappa Hospital and Research Centre, Tamaka, Kolar. The duration of the study was three years (August 2013 to August 2016)[11]. Ethical Clearance was obtained from Institutional Ethics Committee of Sri Devaraj Urs Medical College. The study population enrollment was commenced after obtaining patient written informed consent. The study was conducted in collaboration with Department of Obstetrics and Gynecology.
All pregnant women after 20 weeks of gestation with preeclampsia diagnosed as per National High Blood Pressure Education Programme working group (NHBPEP) classification admitted with singleton pregnancy, no fetal anatomical anomaly, nonsmokers were included in the study at R L Jalappa Hospital and Research Center. Pre-eclampsia was diagnosed with blood pressure of ≥140/90 mm of Hg noted for the first time during pregnancy on ≥2 occasions at least 4 hours apart, after 20 weeks of gestation with proteinuria of ≥300 mg/24 hours or ≥ 1+. History of renal disease, history of thyroid disorder, history of chronic hypertension, history of gestational diabetics, history of epilepsy, history of hypertensive encephalopathy, history of cardio vascular disease and multigravida were excluded. 50 preeclamptic women and 50 normotensive pregnant women in the third trimester and age between 18-35 were included in the study.
Four ml of blood was collected and aliquoted from the non-pregnant, normotensive pregnant and preeclamptic women visited department of obstetrics and gynecology. Blood samples were collected and centrifuged at 3000 rpm for 10 minutes to obtain the clear plasma and serum. Thus, obtained clear sera and plasma were stored at -80 ˚C until analysis.
Protein in random urine was estimated by dipstick method. Gamma glutamyl transferase activity was determined by a coupled enzyme assay, in which Gamma glutamyl transferase transfers the Gamma glutamyl group from the substrate L-Gamma glutamyl-p-nitroanilide releasing the chromogen p-nitroanilide. The chromogen p-nitroanilide was measured colorimetrically at 418nm. The intensity of the colour is directly proportional to the amount of the GGT present. Lactate dehydrogenase was measured by spectrophotometric method where lactate is converted to pyruvate with simultaneous reduction of NAD to NADH which was measured colorimetrically at 450nm.
Statistical analysis
The results were expressed as mean ± SD. P value<0.05 was considered as statistically significant. Independent‘t’ test were used to compare the means.
Result
The demographic characteristics such as age distribution of the normotensive pregnant and preeclampsia were depicted in percentage. [Table 1] shows that 25% of the normal pregnant population were in the 18-20 age group and 24% had preeclampsia. In 21-25 age group 56% were normotensive pregnant and 51% were in preeclampsia group.26-30 age group 17% were normotensive and 16% were in preeclampsia with age group more than 30, 2% were in normotensive and 9% had preeclampsia.
| Age in years | Normotensive pregnant (n=50) | Preeclampsia (n=50) |
| Percentage | Percentage | |
| 18-20 | 25 | 24 |
| 21-25 | 56 | 51 |
| 26-30 | 17 | 16 |
| >30 | 2 | 9 |
| Gestational age in weeks | Normotensive pregnant (n=50) | Pre-eclampsia (n=50) | |
| Percentage | Percentage | ||
| 28-33 | 4 | 16 | |
| 34-37 | 14 | 25 | |
| 38-40 | 82 | 59 | |
| >40 | 0 | 0 |
The distribution of gestational age for the subjects of normotensive pregnant and preeclampsia were represented as percentage. Gestational week between 34-37 shows 14% ormotensive and 25% preeclamptic. Gestational week between 38-40 week had 82% normotensive and 59% preeclampsia.
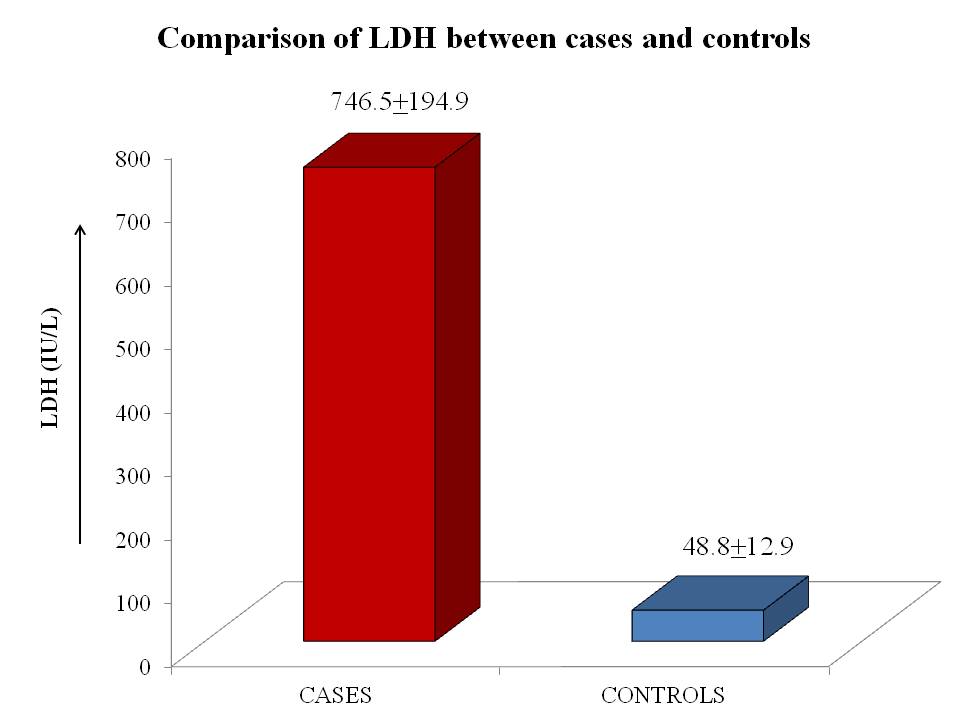
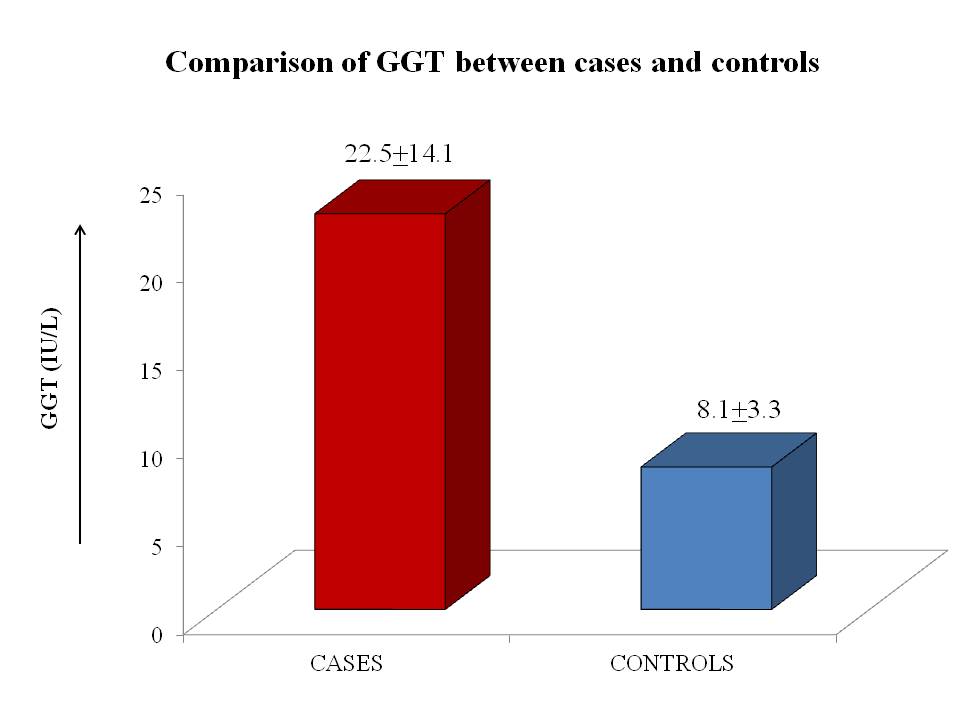
[Table 3] shows that systolic blood pressure, diastolic blood pressure, LDH and GGT had P value<0.001. Haemoglobin has not showed significance between normal pregnant women and preeclampsia levels between mild and severe preeclampsia.
| Parameters | Normotensive pregnant women (n= 50) MEAN ± SEM | Preeclamptic women (n= 50 ) MEAN ± SEM | Significance |
| Systolic blood pressure (mm/Hg) | 116.67± 1.20 | 159.03 ± 2.98 ** | <0.001 |
| Diastolic blood pressure(mm/Hg) | 86.67± 1.04 | 100.32± 1.99 ** | <0.001 |
| LDH (IU/L) | 48.8± 1.96 | 746.5± 35.6 ** | <0.001 |
| GGT (IU/L) | 8.09 ±0.50 | 22.5± 2.5 ** | <0.001 |
| Haemoglobin(gm/dl) | 11.0951 ± 0.34 | 11.4179 ± 0.44 | >0.5 |
Discussion
Our finding shows that women with more than 30 age groups are at increased risk of getting preeclampsia compared to the normal pregnant women. Previous studies reported teenage pregnancy and increased maternal age increases risk of preeclampsia.[12] We found preterm delivery is the major consequence of preeclampsia which goes with literature.[13] Odul AA et al showed high maternal haemoglobin concentration in normotensive women associated with IUGR. But in our studies we found no difference in haemoglobin levels in normotensive pregnant women and preeclampsia.[14]
GGT and LDH significantly increased in preeclampsia group when compared to normal pregnant women.[13] Study conducted by Amburgey showed increase in haemoglobin levels in preeclampsia but in the present study found no change in haemoglobin levels.[15],[16]
Normal placentation involves extensive implantation of spiral arterioles which were invaded by endovascular trophoblast that replaces vascular endothelial and muscular linings leading to the enlargement of the vessel diameter. Abnormal placentation involves incomplete trophoblastic shallow invasion which fails to replace vascular endothelial cell and muscular linings. The defective trophoblastic invasion leads to the constriction of spiral arteries and diminish the vessel diameter compare to normal placentation. Thus, leads to the varied oxygenation in placenta generating free radicals and oxidative stress. As compensatory mechanism to hypo perfusion and oxidative stress, placenta releases factors in to the circulation which may results in systemic alterations.[17],[18] Ischemic placenta contributes to the endothelial dysfunction by altering circulating levels of angiogenic and antiangiogenic factors. Endothelial cell dysfunction may be also due to activated leukocytes by cytokines which adds to the oxidative stress and destructs the endothelial cells.[19],[20] In preeclampsia, cellular dysfunction leads to the LDH leakage to the extracellular space. GGT is a microsomal enzyme its levels increases in hepatic injury.[21] However in the current study the increased GGT levels shows that not only by hepatic origin but its levels are a lso increased in tissue damage in preeclampsia.
Conclusion
In preeclampsia, vascular endothelial damage may lead to multi organ dysfunctions leads to excessive LDH leakage and elevated levels in serum due to cellular dysfunction. GGT is increased in hepatic injury, however in the current study the increased GGT levels shows that not only by hepatic origin but its levels are also increased in tissue damage during preeclampsia as a major cause of endothelial vascular damage. Elevated levels of serum LDH and serum GGT indicates the tissue damage related to endothelial vascular damage and is the main cause of preeclampsia.
Limitations
The present study limits in the analysis of the LDH and GGT from the time of pregnancy to delivery in preeclampsia in comparison with normal pregnant women which is useful in developing cut-off values.
Acknowledgments
Thanks to the staff of the Department of Biochemistry, SDUMC, Kolar.
Conflict of interest
None declared.
References
- J M Roberts, Cwg Redman. Pre-Eclampsia: More than pregnancy induced hypertension. Lancet 1993. [Google Scholar]
- 2. Siaai BM .. Hypertensive disorders of pregnancy: the United States prospective. Curr Opin Obstet Gynecol 2008. [Google Scholar]
- . Gabor Than award lecture 2008: preeclampsia-From placental Oxidative stress to maternal endothelial dysfunction. Placenta 2009. [Google Scholar]
- P Dadleszen, - Mageela, E L Taylor, J C Muir, S D Stewart. Maternal hypertension and neonatal outcome among small for gestational age infants. Obstect Gynecol 2005. [Google Scholar]
- A Rubina, M Tabassum. Relation between preeclampsia and cardiac enzymes. ARYA Atheroscler 2007. [Google Scholar]
- P Dadelszen, L A Magee, E L Taylor, J C Muir, S D Stewart, P Sherman. Maternal hypertension and neonatal outcome among small for gestational age infants. Obstet Gynecol 2005. [Google Scholar]
- V Kumar, A K Abbas, N Fausto. . Robbins and Cotran pathologic basis of disease. 7th ed 2005. [Google Scholar]
- C Henderson, S Macdonald. . A textbook for midwives.13th ed 2004. [Google Scholar]
- T Y Khong, F De Wolf, W B Robertson, I Brosens. Inadequate maternal vascular response to placentation in pregnancies complicated by preeclampsia and by small for-gestational age infants. Br J Obstet Gynaecol 1986. [Google Scholar]
- S M Munde, N R Hazari, A P Thorat, S B Gaikwad, V S Hatolkar. Gamma Glutamyl Transferase and Lactate dehydrogenase as biochemical markers of severity of preeclampsia. Int Sci Index 2014. [Google Scholar]
- N S Bakhshandeh, R Azarhoosh, A Borghei, M Sedaghati, Besharat. Serum level of lactate dehydrogenase, homocystein, hemoglobin, and platelet in preeclampsia. Pak J Med Sci 2011. [Google Scholar]
- Y Bdolah, G E Palomaki, Y Yaron, A T Bdolah, M Goldman, R J Levine. Circulating angiogenic proteins in trisomy 13. Am J Obstet Gynecol 2006. [Google Scholar]
- A Odul Amburgey, EliesaIng, J Gary Badger, M Ira Bernstein. Maternal Hemoglobin Concentration and its Association with. J Matern Fetal Neonata 2009. [Google Scholar]
- O A Amburgey, E Ing, G J Badger, I M Bernstein. Maternal hemoglobin concentration and its association with birth weight in newborns of mother with preeclampsia. J Matern Fetal Neonatal Med 2009. [Google Scholar]
- Abdel Azeim Ali, A Duria Rayis, M Tajeldin Abdallah, I Mustafa Elbashir, Ishang Adam. Severe anemia is associated with a higher risk for preeclampsia and poor perinatal outcomes in Kassala hospital, eastern Sudan. BMC Research Notes 2011. [Google Scholar]
- S E Salih Ezzaldein, Abdelgadir Eltom, L Ahmed Osman, M A Asaad Babker. -. Int J Reprod Contracept Obstet Gynecol 2018. [Google Scholar]
- R Madazli, E Budak, Z Calay, M F Aksu. Correlation between placental bed biopsy findings, vascular cell adhesion molecule and fibronectin levels in preeclampsia. BJOG 2000. [Google Scholar]
- C W Redman, I L Sargent. Latest advances in understanding preeclampsia. Science 2005. [Google Scholar]
- N S Bakhshandeh, R Azarhoosh, A Borghei, M Sedaghati, Besharat. Serum level of lactate dehydrogenase, homocystein, hemoglobin, and platelet in preeclampsia. Pak J Med Sci 2011. [Google Scholar]
- Y Bdolah, G E Palomaki, Y Yaron, A T Bdolah, M Goldman, R J Levine. Circulating angiogenic proteins in trisomy 13. Am J Obstet Gynecol 2006. [Google Scholar]
